Guillain-Barré Syndrome (GBS) is a rare, yet serious, neurological disorder that can progress rapidly. Imagine waking up one day with a tingling sensation in your toes, only to find that within hours or days, your muscles feel weak and unresponsive. This article is designed to help you recognize the early warning signs of GBS, debunk common myths, and understand why early detection is crucial for effective treatment.
Introduction
Have you ever experienced an unexpected, unexplained weakness in your legs or arms? For many, such symptoms might be brushed off as fatigue or a minor injury. However, when these signs appear suddenly and progress quickly, they might signal something more serious. Guillain-Barré Syndrome, though rare, can escalate swiftly, making early detection vital. This article will walk you through the warning signs of GBS, provide expert insights, and offer actionable advice on what to do if you or a loved one experiences these symptoms.
Table of Contents
What Is Guillain-Barré Syndrome?
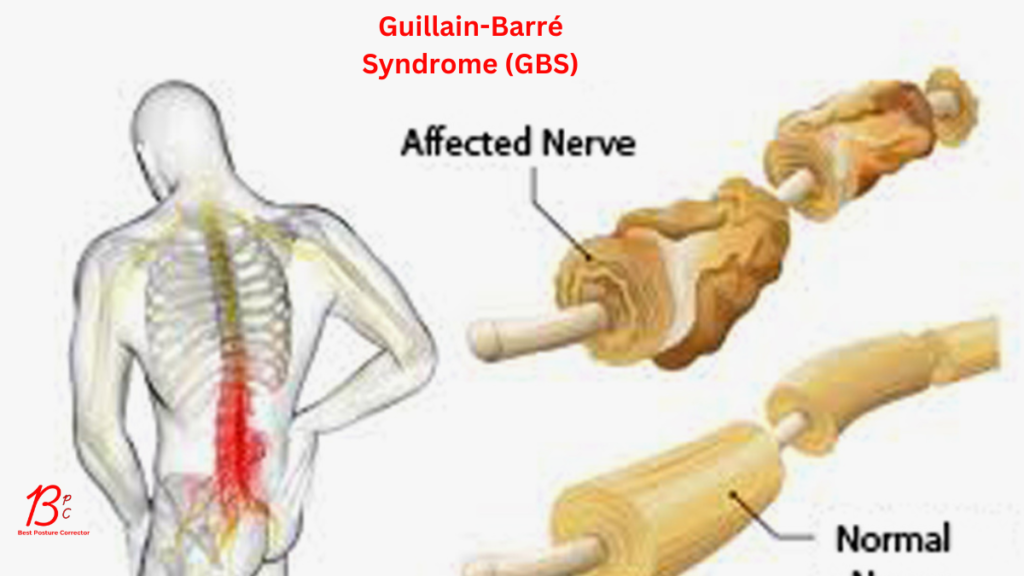
Guillain-Barré Syndrome is a rare autoimmune condition in which the immune system wrongly targets the peripheral nerves. This can lead to inflammation and damage, resulting in symptoms that range from mild weakness to complete paralysis. Although the exact cause is unknown, GBS often follows an infection, such as a respiratory or gastrointestinal illness.
Key Points:
- Autoimmune Response: The immune system targets the peripheral nervous system.
- Rapid Progression: Symptoms can worsen quickly, sometimes within days.
- Variable Impact: Ranges from minor muscle weakness to life-threatening paralysis.
The Importance of Early Detection
Early detection of Guillain-Barré Syndrome can make a significant difference in outcomes. When GBS is identified in its initial stages, treatments such as intravenous immunoglobulin (IVIG) or plasmapheresis can be administered to help slow the progression and reduce complications. Delay in diagnosis, however, may lead to severe outcomes, including respiratory failure and long-term disability.
Why Early Detection Matters:
- Prevents Severe Complications: Quick intervention can mitigate the risk of respiratory failure.
- Improves Recovery Chances: Early treatment increases the likelihood of a full or near-full recovery.
- Reduces Hospitalization Time: Timely management can shorten the duration of hospital stays and rehabilitation.
Recognizing the Warning Signs
GBS presents a range of symptoms, many of which may initially seem benign. Recognizing these early signs is crucial. Here are the most common warning signals:
1. Progressive Weakness
One of the hallmark signs of GBS is a gradual onset of muscle weakness that often starts in the legs and ascends upward.
- Early Stage: You might notice difficulty climbing stairs, getting up from a seated position, or walking.
- Advanced Stage: Weakness may spread to the arms and upper body, eventually affecting the muscles involved in breathing.
Bullet Point Summary:
- Initial Signs: Difficulty walking, tripping, or a noticeable decline in leg strength.
- Warning Indicator: Rapid progression of weakness over days.
2. Tingling Sensations and Numbness
Patients frequently report a sensation of “pins and needles” or numbness, particularly in the hands and feet.
- Early Stage: These sensations might be intermittent and mild.
- Progression: The feelings can intensify, leading to significant discomfort and loss of sensation.
Visual Suggestion: A diagram showing areas of the body commonly affected by tingling and numbness in GBS patients.
3. Coordination and Balance Issues
As the syndrome progresses, impaired coordination can make routine tasks challenging.
- Symptoms Include: Clumsiness, unsteadiness, and difficulty maintaining balance.
- Impact on Daily Life: These issues may lead to falls and other injuries, especially in older adults.
4. Respiratory Difficulties
When GBS affects the muscles responsible for breathing, it becomes a medical emergency.
- Warning Signs: Shortness of breath, difficulty breathing deeply, or labored breathing.
- Critical Stage: Respiratory failure can occur, necessitating immediate intervention and possibly mechanical ventilation.
5. Autonomic Dysfunction
In some cases, GBS can disrupt the autonomic nervous system, which controls involuntary body functions.
- Symptoms Include: Irregular heartbeats, fluctuations in blood pressure, and digestive issues.
- Note: These symptoms may be subtle at first but can worsen rapidly.
6. Other Potential Signs
Other symptoms might include:
- Severe Pain: Often described as aching or cramping, primarily in the lower back.
- Facial Weakness: Difficulty with facial expressions or swallowing.
- Visual Disturbances: Blurred or double vision, although less common.
Bullet Point Summary:
- Progressive weakness and tingling.
- Difficulty with coordination and balance.
- Respiratory challenges.
- Signs of autonomic dysfunction.
- Severe pain and facial weakness.
Debunking Common Myths About Guillain-Barré Syndrome
With any rare condition, misconceptions can spread quickly. Here are some common myths about GBS, along with the facts:
- Myth 1: GBS is Highly Contagious.
Fact: GBS is not contagious. It is an autoimmune response, often triggered by an infection, but it cannot be passed from person to person. - Myth 2: Only the Elderly Are Affected.
Fact: While older adults may face more severe complications, GBS can affect individuals of all ages, including children and young adults. - Myth 3: Recovery Is Rare.
Fact: Many patients recover fully or near-fully with prompt treatment. Early detection and intervention are key.
Visual Suggestion: A myth vs. fact chart to help clarify these common misconceptions.
What to Do if You Suspect GBS
If you or someone you know exhibits these warning signs, it’s important to take action promptly:
- Seek Medical Attention Immediately:
Don’t wait for symptoms to worsen. A healthcare provider can perform tests such as nerve conduction studies or a lumbar puncture to confirm the diagnosis. - Document Your Symptoms:
Keep a record of any changes in strength, sensation, or coordination. This information can be invaluable during medical evaluations. - Consult a Specialist:
A neurologist, who specializes in disorders of the nervous system, will be best equipped to diagnose and manage GBS. - Follow Medical Advice:
Early intervention with treatments like IVIG or plasmapheresis can significantly improve outcomes. Adhering to your healthcare provider’s recommendations is essential.
Bullet Point Summary:
- Act quickly by seeking professional help.
- Document and monitor symptoms.
- Consult with a neurologist.
- Adhere to treatment plans for better recovery prospects.
Expert Insights and Case Studies
Dr. Jane Smith, a neurologist at a leading medical center, emphasizes, “Recognizing the early signs of Guillain-Barré Syndrome can be life-saving. Patients often describe their initial symptoms as minor inconveniences, but these should never be ignored.”
A study published in the New England Journal of Medicine highlighted that patients who received treatment within the first week of symptom onset had significantly better outcomes compared to those with delayed treatment. Such research reinforces the importance of early detection and intervention.
Source Links:
Visual Suggestion: A sidebar featuring a brief interview or quote from a medical expert on the importance of early detection in GBS cases.
Living with Guillain-Barré Syndrome: A Fresh Perspective
While the diagnosis of Guillain-Barré Syndrome can be daunting, many patients go on to lead fulfilling lives. Rehabilitation plays a crucial role in recovery, focusing on regaining strength, mobility, and confidence. Today’s advancements in physical therapy and neurological care have transformed the outlook for many GBS patients.
Key Takeaways for Living with GBS:
- Rehabilitation Is Key: Intensive physical therapy can help restore function.
- Mental Health Matters: Coping with a sudden loss of mobility can be challenging. Support from mental health professionals, family, and peer groups is essential.
- Community and Resources: Numerous support groups and resources are available for patients and their families to share experiences and tips for recovery.
Visual Suggestion: An image of a support group session or a rehabilitation center, highlighting the community aspect of recovery.
Conclusion
Guillain-Barré Syndrome is a complex condition, but understanding its early warning signs can make all the difference. From progressive weakness and tingling sensations to respiratory difficulties and autonomic dysfunction, recognizing these symptoms is the first step toward effective treatment. As research and medical advancements continue to improve outcomes, early detection remains the cornerstone of a successful recovery.
Call to Action:
If you or someone you know experiences any of these warning signs, do not hesitate—seek medical advice immediately. Early intervention can save lives and pave the way for a better quality of life. How might recognizing these symptoms earlier change your perspective on your health and that of your loved ones?
By staying informed and vigilant, you empower yourself and your community to act quickly and decisively when it matters most.
SEO Keywords Recap: Guillain-Barré syndrome, early warning signs, neurological disorder, progressive weakness, tingling sensations, early detection.
For further reading and trusted medical insights, visit reputable sources like the Mayo Clinic and the Centers for Disease Control and Prevention.